External radiotherapy for vaginal cancer
Radiotherapy uses high energy x-rays to treat cancer cells.
External radiotherapy uses a machine outside the body to direct radiation beams at the cancer to destroy it. It is a common treatment for vaginal cancer.
When do you have it?
You might have radiotherapy for vaginal cancer:
-
as your main treatment
-
to treat vaginal cancer if you can't have surgery
-
to help stop the cancer coming back after surgery
-
to treat vaginal cancer that couldn't be completely removed with surgery
-
as a combination treatment with chemotherapy (chemoradiotherapy)
You go to the hospital for treatment once a day, from Monday to Friday, with a break at the weekends. Each treatment takes around 25 minutes.
The length of your course of treatment varies. This depends on the type and size of your cancer and on the aim of the treatment.
Where do you have external radiotherapy?
You usually have external radiotherapy in the hospital radiotherapy department as an outpatient. Some hospitals have rooms near the hospital you can stay in if you have a long way to travel. You go to the radiotherapy department from your ward if you’re already in the hospital.
Planning radiotherapy
The radiotherapy team plans your external beam radiotherapy before you start treatment. This means working out the dose of radiotherapy you need and exactly where you need it.
Your planning appointment takes up to 2 hours.
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
Your  tell you what will happen during the planning CT scan.
tell you what will happen during the planning CT scan.
Before the scan
Before the scan you need to empty your bowels. Your radiographer might give you an  to help you empty your bowels. You will also need to drink a certain amount of water before you have the scan. They will tell you how much.
to help you empty your bowels. You will also need to drink a certain amount of water before you have the scan. They will tell you how much.
You may need to prepare your bowels and bladder in the same way before each treatment. This helps to improve the accuracy of the treatment and reduce the possible side effects.
Your radiographer will ask you to put on a hospital gown. When you’re ready, the radiographers help you to position yourself on the scanning couch. This is the same type of bed that you lie on for your treatment sessions.
You need to lie very still. You might have a type of firm cushion called a vacbag to help as you may be in this position for a little while. Let the radiographers know if you are uncomfortable.
Injection of dye
You might need an injection of  through a small thin tube (cannula) in your arm.
through a small thin tube (cannula) in your arm.
Before you have the contrast medium, the radiographer asks you about any medical conditions or allergies. Some people are allergic to the dye.
For some people the dye might:
- make you feel hot and flushed for a minute or two
- give you a metallic taste in your mouth, but this will not last long
- make you feel like you’re passing urine but you aren’t. This feeling usually passes quickly
Having the scan
Once you're in a comfortable position the radiographers move the couch up and through the scanner. They then leave the room and the scan starts.
The scan takes about 20 minutes. You won't feel anything. The radiographers can see you from the CT control area where they operate the scanner.
Ink and tattoo marks
The radiographers make pin point sized tattoo marks on your skin. They use these marks to line you up into the same position every day. The tattoos make sure they treat exactly the same area for all of your treatments. They may also draw marks around the tattoos with a permanent ink pen, so that they are clear to see when the lights are low.

The radiotherapy staff tell you how to look after the markings. The pen marks might start to rub off in time, but the tattoos won’t. Tell your radiographer if that happens. Don't try to redraw them yourself.
After the scan
The radiographers will help you off the CT scanner couch and you can get changed back into your clothes. You stay in the department for about 15 to 30 minutes if you had an injection of the dye. This is in case it makes you feel unwell, which is rare.
The radiographer removes the tube from the vein in your arm before you go home.
You should be able to go home or back to work. You can eat and drink normally.
After your planning session
You might have to wait a few days or up to 3 weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan. They make sure that the area of the cancer will receive a high dose and nearby areas receive a low dose. This reduces the side effects you might get during and after treatment.
Having external radiotherapy
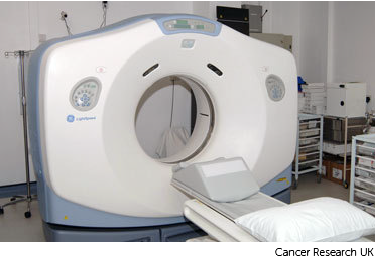
Radiotherapy machines are very big and could make you feel nervous when you see them for the first time. The machine might be fixed in one position. Or it might rotate around your body to give treatment from different directions. The machine doesn't touch you at any point.
Before your first treatment, your  will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.
will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.

Before your treatment
Before each treatment you need to empty your bowels. Your radiographer might give you an enema to help you.
You will also need to drink a certain amount of water before treatment. They will tell you how much, and when to drink it.
During the treatment
You need to lie very still. Your radiographers might take images (x-rays or scans) before your treatment to make sure that you're in the right position. The machine makes whirring and beeping sounds. You won’t feel anything when you have the treatment.
Your radiographers can see and hear you on a CCTV screen in the next room. They can talk to you over an intercom and might ask you to hold your breath or take shallow breaths at times. You can also talk to them through the intercom or raise your hand if you need to stop or if you're uncomfortable.
You won't be radioactive
This type of radiotherapy won't make you radioactive. It's safe to be around other people, including pregnant women and children.
Travelling to radiotherapy appointments
You might have to travel a long way each day for your radiotherapy. This depends on where your nearest cancer centre is. This can make you very tired, especially if you have side effects from the treatment.
You can ask your radiographers for an appointment time to suit you. They will do their best, but some departments might be very busy. Some radiotherapy departments are open from 7 am till 9 pm.
Car parking can be difficult at hospitals. Ask the radiotherapy staff if you are able to get free parking or discounted parking. They may be able to give you tips on free places to park nearby.
Hospital transport may be available if you have no other way to get to the hospital. But it might not always be at convenient times. It is usually for people who struggle to use public transport or have any other illnesses or disabilities. You might need to arrange hospital transport yourself.
Some people are able to claim back a refund for healthcare travel costs. This is based on the type of appointment and whether you claim certain benefits. Ask the radiotherapy staff for more information about this and hospital transport.
Some hospitals have their own drivers and local charities might offer hospital transport. So do ask if any help is available in your area.
Side effects
Radiotherapy for vaginal cancer can cause loose poo (diarrhoea), sickness, and tiredness. Many side effects usually go away within a few weeks of finishing treatment.



