A trial comparing electronic cigarettes with nicotine replacement therapy to stop smoking (TEC)
Cancer type:
Status:
Phase:
The trial compared electronic cigarettes with nicotine replacement therapy. To determine if e-cigarettes were as helpful or more helpful in assisting with stopping smoking.
People who want to reduce the risks of smoking might choose electronic cigarettes. Because they:
- copy the action of smoking
- are much safer than conventional cigarettes
This trial was open for people to join between May 2015 and February 2018. These results were published in 2019.
More about this trial
People wishing to stop smoking can use nicotine replacement therapy. This involves using a product, such as nicotine gum or a patch, to give nicotine.
We know that electronic cigarettes can reduce the urge to smoke. What we didn’t know was whether they were as good as nicotine replacement therapy at helping people to quit smoking.
This trial compared electronic cigarettes with nicotine replacement therapy. Half the people used electronic cigarettes. The other half used nicotine replacement therapy. Both groups also had support to help them with stopping smoking.
The aims of the trial were to:
- find out if electronic cigarettes were better than nicotine replacement therapy to help people quit smoking
- compare the side effects of the 2 treatments
Summary of results
The trial found that electronic cigarettes (e-cigarettes) worked better than nicotine replacement therapy.
About this trial
This was a randomised trial. Everyone was put into 1 of 2 groups. Neither they nor their doctor chose which group they were in.
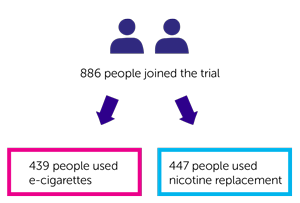
886 people joined the trial:
- 439 people used e-cigarettes
- 447 people used nicotine replacement
People in the e-cigarette group had an e-cigarette starter pack. It contained:
- a refillable e-cigarette
- instructions on how to use it
- a bottle of e-liquid to start them off
People in the nicotine replacement group had information about the range of products available. They could choose which product or products they wanted to use.
Results
Of the 439 people in the e-cigarette group they were able to look at the results of 438.
Of the 447 people in the nicotine replacement group they were able to look at the results of 446.
After a year the team looked at how many people in each group were still not smoking (abstained). They found it was:
- 79 people (18%) in the e-cigarette group
- 44 people (9.9%) in the nicotine replacement group
They also looked at the number of people who were still using their e-cigarette or nicotine replacement. They found it was:
- 173 people (39.5%) in the e-cigarette group
- 19 people (4.3%) in the nicotine replacement group
The team looked at the frequency and strength of urge to smoke 1 week and 4 weeks after quitting smoking. They found it was greater for people in the nicotine replacement group.
They also looked at the difference in lung symptoms such as:
- shortness of breath
- wheezing
- coughing
- phlegm produced
After a year the coughing and phlegm production had decreased in both groups. But the amount these had decreased by was greater for those in the e-cigarette group.
Side effects
The side effects reported were:
- feeling sick
- problems with sleeping
- irritation of the mouth and throat
More people using e-cigarettes reported mouth and throat irritation. While more people using nicotine replacement treatments reported feeling sick.
Conclusion
The trial team concluded that refillable e-cigarettes helped people to stop smoking better than nicotine replacement treatments.
Where this information comes from
We have based this summary on information from the research team. The information they sent us has been reviewed by independent specialists ( ) and published in a medical journal. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.
) and published in a medical journal. The figures we quote above were provided by the trial team who did the research. We have not analysed the data ourselves.
Recruitment start:
Recruitment end:
How to join a clinical trial
Please note: In order to join a trial you will need to discuss it with your doctor, unless otherwise specified.
Chief Investigator
Professor Peter Hajek
Supported by
Queen Mary University of London
NIHR Health Technology Assessment (HTA) programme
East Sussex Stop Smoking Service
Leicester Stop Smoking Service
Barts Clinical Trials Unit
If you have questions about the trial please contact our cancer information nurses
Freephone 0808 800 4040