Planning external radiotherapy for thyroid cancer
External radiotherapy uses a radiotherapy machine to aim radiation beams at a cancer. This destroys the cancer cells.
The radiotherapy team plan your external radiotherapy before you start treatment. This means working out the dose of radiotherapy you need and exactly where you need it.
Your planning appointment takes from 15 minutes to 2 hours.
The planning CT scan
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
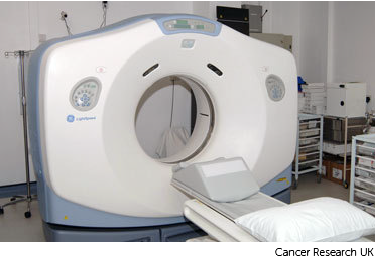
Your radiographers tell you what is going to happen. They help you into position on the scan couch. You might have a type of firm cushion called a vacbag to help you keep still.
The CT scanner couch is the same type of bed that you lie on for your treatment sessions. You need to lie very still. Tell your radiographers if you aren't comfortable.
Injection of dye
You might need an injection of contrast into a vein in your hand. This is a dye that helps body tissues show up more clearly on the scan.
Before you have the contrast, your radiographer asks you about any medical conditions or allergies. Some people are allergic to the contrast.
Having the scan
Once you are in position your radiographers put some markers on your skin. They move the couch up and through the scanner. They then leave the room and the scan starts.
The scan takes about 5 minutes. You won't feel anything. Your radiographers can see and hear you from the CT control area where they operate the scanner.
You lie on the scanner couch with the treatment area exposed.
Watch our video about radiotherapy planning. It is just under 3 minutes long.
Dan (radiographer) : Radiotherapy planning will involve you coming for an appointment for a CT scan in the radiotherapy department. The idea behind this is that the doctor needs to work out exactly where needs to be treated and where we need to avoid and so that scan starts us off on that process.
For the CT scan, most of the time no preparation is needed beforehand but if any is then you’ll receive that in a letter so for example, depending on what you having treated there might need to be a contrast agent introduced or you may need to have a full or an empty bladder depending on what is necessary for the scan. There are a number of things we do to help people keep still and make sure the cancer is treated.
It is important that you lie in the same position every time you have treatment. This is to make sure the radiotherapy is directed at the cancer and normal tissues are avoided. We may put equipment in place to fix your position. If you are having radiotherapy for a head and neck cancer you will have a mask made. The mask helps you to keep your head really still during treatment. We also line up the scanner and mark your skin with a felt pen where the light lines from the machine need to be aimed.
They’ll then leave the room and start the scanner and that scan lasts usually about 2 to 3 minutes. Because pen marks can rub easily the radiographer makes them permanent after your scan by tattooing very small marks on your skin.
After the scan the radiographers will give you any information that you need before starting treatment and answer any questions that you’ve got then you are free to go home.
Patient: When I came for the first meeting to plan the treatment. It was a case of having a scan and then lying, remaining on the scan machine and then the technicians took some measurements some dimensions and when they were satisfied that they had the right angles they tattooed me.
Dan (radiographer): The next part of planning is your doctor looking at the scan and marking out on the computer where you need treatment. Once that’s been done a physicist or a dosimetrist will start to plan your treatment. And they use very powerful computers to work out exactly what dose needs to be given and from which directions it needs to come on from.
Ink and tattoo marks
The radiographers make pin point sized tattoo marks on your skin. They use these marks to line you up into the same position every day. The tattoos make sure they treat exactly the same area for all of your treatments. They may also draw marks around the tattoos with a permanent ink pen, so that they are clear to see when the lights are low.

The radiotherapy staff tell you how to look after the markings. The pen marks might start to rub off in time, but the tattoos won’t. Tell your radiographer if that happens. Don't try to redraw them yourself.
Radiotherapy mask (mould)
Your treatment team might make a mask for you if you are having radiotherapy to your head and neck area. They are also called radiotherapy shells.
Your treatment team will make one for you to wear during your treatment sessions. It will help you to keep very still when you have radiotherapy.
The radiographers make marks on the mask and use the marks to line up the radiotherapy machine for each treatment.
The process of making the shell can vary slightly between hospitals. It usually takes around 30 minutes.
Before making the mask
You need to wear clothes that you can easily take off from your neck and chest. You also need to take off any jewellery from that area.
Facial hair, long hair or dreadlocks can make it difficult to mould the shell. The radiotherapy staff will tell you if you need to shave or to tie your hair back.
Making the mask
A technician uses a special kind of plastic that they heat in warm water. This makes it soft and pliable. They put the plastic on to your face, neck and chest so that it moulds exactly.
After a few minutes the plastic gets hard. The technician takes the mask off and it is ready to use.

After your planning session
You might have to wait a few days or up to 3 weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan. They make sure that the area of the cancer will receive a high dose and nearby areas receive a low dose. This reduces the side effects you might get during and after treatment.



