Radiotherapy for vulval cancer
Radiotherapy uses high energy x-rays to treat cancer cells. For vulval cancer, you usually have external radiotherapy. This means using a radiotherapy machine to aim radiation beams at the cancer.
You have this treatment in the hospital radiotherapy department. It doesn't hurt, although laying on the radiotherapy couch can be uncomfortable. You are most likely to have treatment once a day, Monday to Friday, with a rest at the weekends. You usually have treatment for 5 to 6 weeks.
When you might have radiotherapy for vulval cancer
You usually have radiotherapy after surgery to remove vulval cancer. This is called adjuvant treatment. You may also have it:
- before surgery
- instead of surgery
- to control symptoms
- as a radiation boost at the end of your main radiotherapy treatment
You may have radiotherapy on its own or in combination with chemotherapy. This is chemoradiotherapy.
Your doctors may recommend you have radiotherapy after surgery if there is a high risk of the cancer coming back. Radiotherapy can kill off any cancer cells that might have been left behind after your operation.
You may have treatment to the groin on one or both sides, depending on where the cancer was. You may also have radiotherapy to the lymph nodes in the pelvic area.
You may also have radiotherapy after surgery if it was not possible to remove all of your vulval cancer. This can happen when the cancer is too close to other important parts of your body. For example, your back passage (anus) or the tube that drains your bladder (the urethra).
Doctors call this neo adjuvant treatment. The aim of radiotherapy before surgery is to shrink your cancer so you can have a smaller operation. Or it may make surgery possible when it wasn't before.
You may have radiotherapy instead of surgery if you can't have surgery for any reason. This might be because:
- you are not well enough for an anaesthetic, or to make a good recovery from the operation
- it is not possible to remove the cancer by surgery
In advanced vulval cancer, the vulval area can sometimes break down and form a wound. The wound may ooze an unpleasant discharge that can smell and be painful. You may hear this called a fungating wound. They can happen in many different types of cancer.
Your nurse can help you to manage the wound with special dressings that can absorb the discharge and help control any smell.
Radiotherapy can also help with fungating wounds. It can shrink the cancer and stop the discharge. The area may even heal completely over time.
You may have a radiation boost at the end of your main radiotherapy treatment. The boost gives a higher dose of treatment, to a smaller part of the treatment area. You may have the boost treatment as external radiotherapy, or as internal radiotherapy.
Internal radiotherapy means having radiation treatment from inside the body. This is also called brachytherapy.
Types of radiotherapy for vulval cancer
You usually have external radiotherapy. This means that a radiotherapy machine aims the radiation beams at the cancer.
There are different types of external radiotherapy. Your doctor decides which is best for you.
You are most likely to have conformal radiotherapy or intensity modulated radiotherapy (IMRT). These shape the radiation beams to closely fit the area of the cancer.
You may also have a boost dose of internal radiotherapy.
Internal radiotherapy means having a very high dose of radiotherapy on or very near the cancer. You may also hear doctors calling this brachytherapy.
You have internal radiotherapy using an implant or a mould.
You have implants put in under general anaesthetic. While you are asleep the doctor puts thin hollow tubes (applicators) into the skin of the vulva. The applicators stay in for 2 to 3 days while you have treatment. You stay in the ward, then go to the radiotherapy department for each treatment.
At the start of each treatment, the radiographer connects the applicators to a machine. This delivers the radiotherapy directly to the area through the applicators. When you finish all your treatment the applicators are removed.
You may also have internal radiotherapy using a mould of your vulva. The mould is put in position for each treatment. The applicators attach to the mould to deliver the radiotherapy. The mould is then removed after each treatment.
You usually have 3 to 4 treatments and may have 2 in one day. Each treatment takes about 15 to 20 minutes. Depending on the type of treatment you have you may have this as an inpatient or outpatient.
Planning your radiotherapy treatment
The radiotherapy team plan your external radiotherapy before you start treatment. This means working out the dose of radiotherapy you need and exactly where you need it.
Your planning appointment takes from 15 minutes to 2 hours.
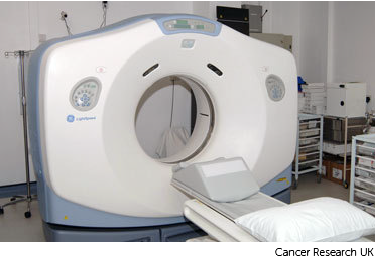
You usually have a planning CT scan in the radiotherapy department.
The scan shows the cancer and the area around it. You might have other types of scans or x-rays to help your treatment team plan your radiotherapy. The plan they create is just for you.
The radiographers tell you what is going to happen. You might need to drink a certain amount of water before you have the scan so that you have a comfortably full bladder. They will tell you how much.
Your radiographers help you into position on the scan couch. You might have a type of firm cushion called a vacbag to help you keep still.
The CT scanner couch is the same type of bed that you lie on for your treatment sessions. You need to lie very still. Tell your radiographers if you aren't comfortable.
Injection of dye
You might need an injection of contrast into a vein in your hand. This is a dye that helps body tissues show up more clearly on the scan.
Before you have the contrast, the radiographer asks you about any medical conditions or allergies. Some people are allergic to the contrast.
Having the scan
Once you are in position the radiographers put some markers on your skin. They move the couch up and through the scanner. They then leave the room and the scan starts.
The scan takes about 5 minutes. You won't feel anything. The radiographers can see you from the CT control area where they operate the scanner.
Ink and tattoo marks
The radiographers make pin point sized tattoo marks on your skin. They use these marks to line you up into the same position every day. The tattoos make sure they treat exactly the same area for all of your treatments. They may also draw marks around the tattoos with a permanent ink pen, so that they are clear to see when the lights are low.
The radiotherapy staff tell you how to look after the markings. The pen marks might start to rub off in time, but the tattoos won’t. Tell your radiographer if that happens. Don't try to redraw them yourself.
After your planning session
You might have to wait a few days or up to 3 weeks before you start treatment.
During this time the physicists and your radiotherapy doctor (clinical oncologist) decide the final details of your radiotherapy plan. They make sure that the area of the cancer will receive a high dose and nearby areas receive a low dose. This reduces the side effects you might get during and after treatment.
The radiotherapy room
Radiotherapy machines are very big and could make you feel nervous when you see them for the first time. The machine might be fixed in one position. Or it might rotate around your body to give treatment from different directions. The machine doesn't touch you at any point.
Before your first treatment, your  will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.
will explain what you will see and hear. In some departments, the treatment rooms have docks for you to plug in music players. So you can listen to your own music while you have treatment.

During the treatment
You need to lie very still. Your radiographers might take images (x-rays or scans) before your treatment to make sure that you're in the right position. The machine makes whirring and beeping sounds. You won’t feel anything when you have the treatment.
Your radiographers can see and hear you on a CCTV screen in the next room. They can talk to you over an intercom and might ask you to hold your breath or take shallow breaths at times. You can also talk to them through the intercom or raise your hand if you need to stop or if you're uncomfortable.
The following is a video about radiotherapy for cancer in general.
Dan (radiographer): Before your treatment starts your doctor will need to work out exactly where the treatment needs to go and also which parts need to be avoided by the treatment. To have radiotherapy you lie in the same position as you did for your planning scans. We then line up the machine based on your tattoo marks. It is really important that you stay very, very still when you are having treatment it is also important to let the radiographers know right at the beginning if you are not comfortable so they can adjust your position
Radiographer: Ok all done, we’ll be back in a couple of minutes
Dan (radiographer): We leave the room and control the room from a separate room This is so we aren’t exposed to radiation. Treatment takes a few minutes and you will be able to talk to us using an intercom. We can see and hear you while you are having your treatment and will check that you are ok. When your treatment starts you won’t feel anything; you may hear the machine as it moves around you giving the treatment from different angles. Because we are aiming to give the same treatment to the same part of the body everyday then the treatment process is exactly the same everyday so you shouldn’t notice any difference. You’ll see someone from the team caring for you once a week while you are having treatment they’ll ask how you are and about any side effects.
You won't be radioactive
This type of radiotherapy won't make you radioactive. It's safe to be around other people, including pregnant women and children.
Travelling to radiotherapy appointments
You might have to travel a long way each day for your radiotherapy. This depends on where your nearest cancer centre is. This can make you very tired, especially if you have side effects from the treatment.
You can ask your radiographers for an appointment time to suit you. They will do their best, but some departments might be very busy. Some radiotherapy departments are open from 7 am till 9 pm.
Car parking can be difficult at hospitals. Ask the radiotherapy staff if you are able to get free parking or discounted parking. They may be able to give you tips on free places to park nearby.
Hospital transport may be available if you have no other way to get to the hospital. But it might not always be at convenient times. It is usually for people who struggle to use public transport or have any other illnesses or disabilities. You might need to arrange hospital transport yourself.
Some people are able to claim back a refund for healthcare travel costs. This is based on the type of appointment and whether you claim certain benefits. Ask the radiotherapy staff for more information about this and hospital transport.
Some hospitals have their own drivers and local charities might offer hospital transport. So do ask if any help is available in your area.
Side effects of radiotherapy
Side effects tend to start a week after the radiotherapy begins. They gradually get worse during the treatment and for a couple of weeks after the treatment ends. But they usually begin to improve after around 2 weeks or so.
Your skin might:
- go red or darker in the treatment area
- feel sore, itchy or warm to touch
- become dry and flaky
Do let your radiotherapy team know if you have any of these symptoms. The symptoms usually go away within 2 to 4 weeks of ending the treatment. But your skin might always be slightly darker in that area.
Tips for looking after your skin during radiotherapy:
- Wash or rinse the area with warm water. Showers are preferable to baths.
- Gently dry the skin with a clean towel, or you may prefer to use a hair dryer on a cool setting.
- You can use a moisturiser on the area (but avoid using creams with perfumes). Check with your radiographer if you are unsure, they may be able to give you a soothing gel or recommend a particular type.
- Wear loose fitting clothing made of natural fibres, such as cotton. This can help reduce irritation to the area.
Radiotherapy to the vulval area may cause problems with your bowel or bladder. These include:
- loose poo (diarrhoea)
- pain or burning when you pee
- feeling like you need to empty your bladder soon after going to the toilet
Speak to your nurse or doctor if you have diarrhoea. They can give you anti diarrhoea medicine to help control it. Drinking plenty of water is important when you have diarrhoea because your body can become dehydrated quickly.
Pain or burning when you pee could be due to  . This side effect usually gets better on its own. Drinking plenty of water can help. Do tell your nurse or radiographer if the symptoms continue.
. This side effect usually gets better on its own. Drinking plenty of water can help. Do tell your nurse or radiographer if the symptoms continue.
These side effects usually start to get better within a week or so of finishing treatment. It is possible to get long term bladder and bowel problems after radiotherapy for vulval cancer, but it is rare.
Radiotherapy can affect the vagina and ovaries. If you are still having periods, your ovaries may stop working and you may have an early menopause. If you do get this, it is likely to be permanent. This means that you will no longer be able to have children naturally and will be infertile.
It can be difficult to accept that you may not be able to have children, even if you already have children. Your doctor will talk to you about this before your treatment starts. You may also find it helpful to talk about how you feel to a counsellor.
Menopause can cause symptoms such as:
- feeling emotional
- hot flushes
- sweats
- dry skin and dry vagina
- tiredness
- anxiety and loss of confidence
- thinning bones
These symptoms can be quite intense and can go on for a long time. As with a natural menopause, it is not possible to predict how long they will last.
You may want to take hormone replacement therapy (HRT) to control your menopause symptoms. You can talk to your doctor about this before your treatment starts. They will explain how it works and if is suitable for you.
Your vagina may shrink and lose its ability to stretch. You may also have vaginal dryness. Both of these symptoms are likely to be long term problems after radiotherapy for vulval cancer.
This can cause difficulty with sexual intercourse, which may become painful. There are different creams and lubricants gels available to help with this.
Your doctor or nurse may also suggest you try vaginal dilators. Dilators are smooth cone shaped objects that you put into your vagina to stretch it. They come in sets of different sizes. Your nurse will give you a set of dilators and show you how to use them.

You use dilators with a water soluble lubricating gel. Starting with a small dilator you gently insert it into the vagina and leave for a few minutes before removing it. You usually do this 3 times a week. When you are comfortable doing this, you can start using larger ones until your vagina is stretched enough for you to have sex comfortably.
After your radiotherapy treatment, your doctor will see you for regular follow up appointments. You may need a vaginal examination at these appointments. The dilators help keep your vagina flexible so that the examination is not painful.
Your doctor and specialist nurse will talk to you about using dilators and other ways of coping with this side effect.
Depending on where you have radiotherapy treatment, there is a risk of developing long term swelling in your groin and legs. This is called lymphoedema. This risk increases if you have surgery to remove the lymph nodes in your groin.
Lymphoedema is a build up of  that causes swelling in a part of the body. It can affect one or both legs depending on whether you had radiotherapy to one or both groins.
that causes swelling in a part of the body. It can affect one or both legs depending on whether you had radiotherapy to one or both groins.
Not everyone will get lymphoedema. It is difficult to say who will or will not develop it. It can happen a few months or years after your treatment.
Treating lymphoedema
Lymphoedema is easier to control if treated early. It is important that you are referred to a lymphoedema specialist if you have signs of swelling. This is usually a nurse or physiotherapist.
There are different treatments for lymphoedema. These include specially fitted stockings and manual lymphatic drainage (MLD).
Tips
It is a good idea to:
- Try to protect your legs and feet from sharp objects - don't walk around in bare feet and wear long trousers for gardening.
- Wear insect repellent to reduce the chance of getting bites.
- Take care of all cuts, scratches or bites without delay, by cleaning with antiseptic and covering with a dressing.
- Avoid sunburn.
- Take extra care when cutting your toenails - you should not cut or tear the cuticles.
- Use an electric razor carefully for shaving your legs.
Radiotherapy can cause hair loss around the vulval area (pubic hair). It may grow back, but it might look different, for example it may be thinner. Sometimes it does not grow back at all.
Voice over: Radiotherapy can cause many different side effects, such as tiredness. The side effects you get will depend on the area you're having treatment to.
This video is about the side effects you might have if you are a woman having radiotherapy to the pelvis or abdomen.
Louise: The abdomen, the tummy, can be affected by radiotherapy, but it depends on which particular part of that we are treating as to what side effects you may experience. If we are treating the upper part of your abdomen and we are irritating your stomach, sometimes you can experience a little bit of nausea, potentially a little bit of vomiting.
This would normally start quite early on if it is going to be a problem and the doctor would prescribe you some medication to help with that.
Carla: I felt sick constantly. I was having Complan drinks and smoothies and milkshakes with fruit and things in. Jelly sweets, anything that had got sugar in that I could suck on or chew on.
And ice cream. I know it was like October/November when I had my treatment, but I was having ice cream every day.
Louise: If your bowels are being irritated by the radiotherapy, you may find you end up a little bit more gassy. Flatulence might be a bit of an issue and sometimes you can find you can end up with some diarrhoea.
Carla: I started to get really, really bad diarrhoea. And they were giving me Imodium-type tablets to combat that.
With the wind, the wind's horrible. It's not nice at all, as a lady, to have wind. There’s tablets available that I can take for that.
Louise: If you do find that you are having some issues with your bowels, always consult with the team before you take any action. It might be they recommend you make some small dietary changes to help with this, cutting out foods which are very high in fibre or very spicy foods.
If you're having issues with diarrhoea, they may also recommend some particular medication to help with that.
Some radiation treatments to the pelvis may also cause some irritation to your bladder, so you might find you need to pass urine more regularly. It may also be more urgent with you passing smaller volumes. Sometimes you may find that there's a little pain or discomfort when you're urinating, or you can't fully empty your bladder like you would do normally.
Carla: If I need to go, I need to go, and if I can't go, I've got to have pant-liners in.
Louise: We would highly recommend during your radiotherapy that you stay well hydrated. We would recommend you drink up to 2 litres of water or squash a day to ensure that this happens.
Drinks to avoid would include anything containing caffeine, so any kind of tea or coffee or decaffeinated drinks, fizzy drinks and alcohol as they all naturally aggravate your bladder.
Radiotherapy can unfortunately have an impact on a woman's sex life. This is because you can end up with some vaginal drying and also you can find that the tissues in the vagina can become a little bit tight as a result of the treatment. The radiotherapy team will support you during treatment to help with any of these particular symptoms.
Carla: You're given dilators when you first finish your treatment and you have to use it for 10 minutes every day just to keep the scar tissue from sticking together and causing an obstruction.
Louise: These are little tubes that are inserted into the vagina that just gently help stretch the tissue to prevent any scar tissue from building and any shrinkage of the muscles. We can also give you some lubrication to help with any sexual activity as well. This can help you moving forward with both your sex life, but also with future internal examinations.
Infertility is a possible side effect of radiotherapy. If you are concerned about infertility after treatment, before you do start any radiotherapy, it's best to talk to the team and they can talk you through potential fertility treatments, such as storing your eggs prior to starting treatment.
It's always best to be open with partners when you're going through any kind of treatment, especially as this may have an impact on them too. It means that you can work through the problems together.
Voice over: If you’re experiencing a side effect that hasn't been covered in this video, you can find more information on the Cancer Research UK website.
You may also have more general side effects from radiotherapy. This includes tiredness and sickness.



